As part of our 30th anniversary we asked for nominations from our community to share their pituitary heroes: people who have gone above and beyond for the pituitary community.
We received 70 nominations and our panel of judges then chose our 30 heroes. It was tough to decide as there were many incredible nominees. Our Pituitary Heroes are the people that have given an exceptional contribution to the pituitary community or are working to create a better future. Through this campaign, we want to thank them and celebrate them!
We will be sharing details about each of the 30 heroes throughout the rest of our 30th year. You can read their stories below, or follow us on social media to find out more!
Click on the heroes names to read more about them and their full story.

Risa August
Risa published a book, “The Road Unpaved”, sharing her personal journey with acromegaly. Through her book and cycling trail of 1,845 miles down the Pacific coast of the US, she contributed to raise awareness about pituitary tumours and inspired many others affected by pituitary conditions.

Peter O'Malley
Peter shares his story of being diagnosed with a pituitary tumour at age fourteen and how this has affected his adult life, while learning from his experience not to give up but stay positive and keep going. Peter has been a volunteer for our helpline for many years, being there to listen and support others affected by a pituitary condition.

Robert Brady
Robert is a Volunteer area coordinator for the Ireland support Group in January 2015. He connects and offers support to all newly diagnosed patients and his work has highly contributed to the awareness and support available to people in Ireland, which was previously not as wide as the UK one.

Hannah Mai
Hannah, while battling with her own health issues, has started the Coventry support group and successfully managed to offer others a safe place to meet, connect and find support. She presented her own story on multiple platforms and events, contributing to raising awareness and inspiring many other people.

Sue Jackson
Sue is a chartered psychologist with a special interest in pituitary conditions. She has spoken at multiple online events for our Foundations, she has been heavily involved in research and she has written articles for our magazine, the Pituitary Life, thus contributing to spreading information amongst our community.

Gail Weingartner
Gail has been involved in our Foundation for over 30 years. She has helped create our support groups as we know them today, and she still volunteers as a local support group co-ordinator. Her passion and constant support have helped many others affected by a pituitary condition who had been recently diagnosed and did not know where to turn to.

Miles Levy
Miles Levy is a consultant endocrinologist and Honorary Professor of Clinical Endocrinology at the University of Leicester Hospitals NHS Trust. He has led the initiative to change the name of Diabetes Insipidus to AVP-Deficiency around the world. His research interests include the pituitary and adrenal gland, and genetics of endocrine tumours.

Pat McBride
Pat has been with the Foundation since 1999. While being a patient herself at the same time, she has worked tirelessly at the Foundation, providing information to newly diagnosed members, being on the helpline and running the Liverpool pit pat group. She is known to many, in the field of Endocrinology, volunteers, patients and corporate companies.

Marie Conley
Marie is the leader of a support group for patients with Cushing’s and s the founder of the Conley Cushing’s fund. She shares her story of Cushing’s Disease with humor and resilience, advocating for early diagnosis and supporting patients through her foundation and board positions. She has helped bringing together and supporting people with Cushing’s and she is a strong advocate for those with the disease.

Steve Harris
Steve initiated the Birmingham Pituitary Patient Support Group back in 1995 and headed this very successfully for many years. He has been a Telephone Buddy, proof reader, given website support, taken part in training events, spoken as an ‘expert patient’, attended professional medical seminars and conferences on behalf of the Foundation.
Regardless of sex, prolactin is a hormone that is present in every body and plays a significant role in producing milk. A prolactinoma is a prolactin-producing tumour on the pituitary gland. This is the most common pituitary condition, and can have life changing impacts on fertility and wellbeing.
Throughout October in 2023, we shined a spotlight on prolactinoma by increasing awareness about the impact of prolactin and prolactinoma, sharing up-to-date information and connect people living with high prolactin levels with experts and one another.
We hosted seven online events for people with prolactinoma and their support networks to learn more about prolactin and prolactinoma. Additionally, we hosted a Prolactinoma Support Group Meeting to exchange experiences and a Q&A session specifically for men with prolactinoma, as their journey often looks different to women. In total, over 130 people attended these events, asked questions and shared their personal stories.
Around 90% of attendees thought the events were good or excellent and increased their knowledge of the subject. We are pleased to have held a session specifically for men with a prolactinoma, as often their experience can be different to others.
On social media we shared information and stories about people living with prolactinoma and these were seen over 88,000 times. The website pages for prolactinoma were also viewed 42% more than a normal month.
If you would like to watch the talks for Pituitary Awareness Month, please visit our YouTube channel.
About Prolactinoma
A prolactinoma is the name given to a prolactin-producing tumour on the pituitary gland. This is a benign tumour, and not a brain tumour or cancer. A prolactinoma causes raised prolactin. This hormone stimulates milk production after childbirth, but is also present in men.
Symptoms vary depending on a person’s sex and can include:
- Loss of periods
- Reduced interest in sex
- Vaginal dryness
- Infertility
- Excess breast milk production
- Difficulty getting an erection
- Headaches
- Visual problems
Once diagnosed through blood tests and scans, a prolactinoma can be treated usually through medication. Surgery can be a treatment method to remove the prolactinoma, although this is less common.
During Pituitary Awareness Month, we shared materials and information about the symptoms, diagnosis and treatments of prolactinoma throughout.
Together, we can make a difference by increasing understanding and support for those affected by prolactin-related conditions within the pituitary community.
A history of campaigning
For over 30 years The Pituitary Foundation has been working to raise awareness and bring about change in policy to improve experiences for pituitary patients and their families.
Foundation staff speak out for pituitary patients in the many rare disease networks we are involved with. This includes:
- Clinical Reference Group in England
- Welsh Cross Party Group for Rare Diseases
- Specialised Health Care Alliance
The Foundation keeps up to date by making sure we are aware of policy decisions that we should respond to on behalf of pituitary patients.
We follow the activities of government's policy work, NICE, relevant cross party groups, charity sector organisations' e-bulletins, health boards, other endocrine based organisations, and commissioning bodies.
Some campaigns we are particularly proud of include:
Response to the new Rare Disease Framework
On Saturday 9 January 2021, the UK Government published a new UK Rare Diseases Framework. This document sets out the underpinning themes and priorities for the next five years that must be acted upon if the lives of people with rare diseases are to improve.
NICE Consultations
The Pituitary Foundation registered as a Stakeholder with NICE (National Institute for Health and Care Excellence) in 2017. As a registered stakeholder, we are included on the list of stakeholders when NICE guidelines are being developed. As stakeholders, we are notified when current guidelines are to be updated, and invited to submit comments for consideration in the updated guidelines.
Since 2017, as an organisation we have submitted comments in relation to topics which we consider to be relevant to our pituitary community.
THINK - Adrenal Insufficiency
In 2017 we worked with University Hospitals Bristol NHS Foundation Trust, to encourage all hospitals to have a protocol in place for managing patients with adrenal insufficiency.
Know your insipidus from your mellitus
Our summer 2016 awareness campaign highlighted the importance of desmopressin being a lifesaving medication, and how it is vital not to confuse diabetes insipidus with diabetes mellitus because they have different causes and very different treatments.
Adrenal crisis e-learning module campaign
In 2016, our spring campaign increased the use of the adrenal crisis e-learning modules by ambulance staff, which was developed by North West England Ambulance Service.
Save Our Loos
Pituitary conditions like AVP deficiency (previously diabetes insipidus) can lead to isolation due to patients having to avoid leaving the house to manage symptoms. The Foundation ran a campaign in 2015 where supporters wrote to their local councillor, signed petitions and spread awareness of DI.
Pituitary tumour v brain tumour
The Pituitary Foundation supports the position that pituitary tumours are not brain tumours.
There is a great deal of debate on this subject and we understand that for many pituitary patients the distinction is an important one.
Our medical committee lead our understanding of endocrinology. They are clear that while the pituitary is in close proximity to the brain, it is not part of the brain.
Price hikes of medicines
The Pituitary Foundation does not condone nor support price hikes relating to any medicines. The costs of medicines are of concern to patients and the NHS alike, and there needs to be robust governance around the pricing of medicines.
The Pituitary Foundation also supports awareness being raised around price hikes of medicines so that governance can be improved. We feel that fair pricing of medicines is important to ensure patients have access to the medicines they need.
Unjust price hikes have damaging consequences to the NHS and cause stress to patients who can see there may be difficulties in continuing to receive an essential medication that they rely on.
Personal campaigns and individual circumstances
The Pituitary Foundation cannot support nor take on any personal awareness campaigns within the NHS, other government agencies, or amongst the general public.
We cannot provide individualised case management for patients or family members.
We cannot intervene in any circumstance faced by individual members of our community with anyone, including employers and medical professionals. Nor can we assist members with procuring medical appointments or tests and we cannot evaluate cases and provide expert diagnosis or treatment advice.
Pituitary conditions and ME/Chronic Fatigue Syndrome
For patients with ME or CFS, some of the symptoms they might experience can be non-specific, similarly to symptoms found in pituitary conditions. The reality is that pituitary conditions are relatively rare and there is no conclusive research to indicate a prevalence of pituitary conditions amongst those with ME or CFS. The Pituitary Foundation suggests ME or CFS patients who believe they have a pituitary condition should see their GP to discuss their symptoms and ask for blood tests relating to pituitary function.
Complementary and alternative therapies
The terms complementary and alternative therapies refer to a diverse group of practices and products not considered part of evidence based, conventional medicine. Some alternative medicines or treatments are based on principles and an evidence base that are not recognised by the scientific community.
Therefore, The Pituitary Foundation wishes to remain neutral on the usefulness of complementary and alternative therapies. However, we recognise some practices have been reported to improve the quality of life for some pituitary patients such as relaxation techniques and art for health.
Product endorsement
The Pituitary Foundation does not recommend, endorse nor promote any products, treatments, consultants or companies. Nor do we offer a negative judgement on a product or person. If it is ever appropriate to make a suggestion we would always attempt to offer details of more than one company.
Head injury and pituitary dysfunction
Traumatic brain injury is common. Pituitary dysfunction following this may occur and is a serious consequence. We would therefore advise that you contact your GP if you have any concerns and experience some of the following symptoms: mild headaches, feeling sick, problems concentrating, poor memory, irritability, tiredness, problems sleeping, lack of appetite, sexual and fertility difficulties, depression, an increased thirst and excessive urinating.
The aim of the campaign was to make opticians and the public aware of the importance of eye tests in checking your health – especially for pituitary tumours!
The more opticians who are aware, the more patients can be diagnosed early and avoid the frustrations associated with a long diagnosis.
We also encouraged everyone to hold Go Orange days and simultaneously raised awareness about the symptoms of pituitary.
We had great support from our partnership with Myers La Roche, a company that provides marketing support and practice sales for opticians and optometrists, which helped us drive our message towards the optical industry!
What we acheived
Awareness Month 2017 was the most successful yet as we saw record numbers of participants getting involved in the campaign and the awareness activities we coordinated.
Over 3,000 copies of our optician awareness leaflet were distributed, and campaign details sent to all the main UK Optician headquarters and prominent ophthalmologist colleges and societies.
An amazing 53 Go Orange events were held!
A huge thank you to everyone who donated to our awareness appeal which will keep our campaigns and awareness work going.
We also published regular news articles regarding the campaign on our website and regular social media content. These news stories included various patient stories about being diagnosed by an optician that were written especially for Awareness Month, and these were very popular. There was a terrific response on Facebook this year with over 123,800 people reached.
Overall, optician awareness has been a popular theme for the last twoAwareness Months. As we have made more opticians aware, more patients will hopefully be diagnosed early and avoid the frustrations associated with a long diagnosis.
Raising Awareness
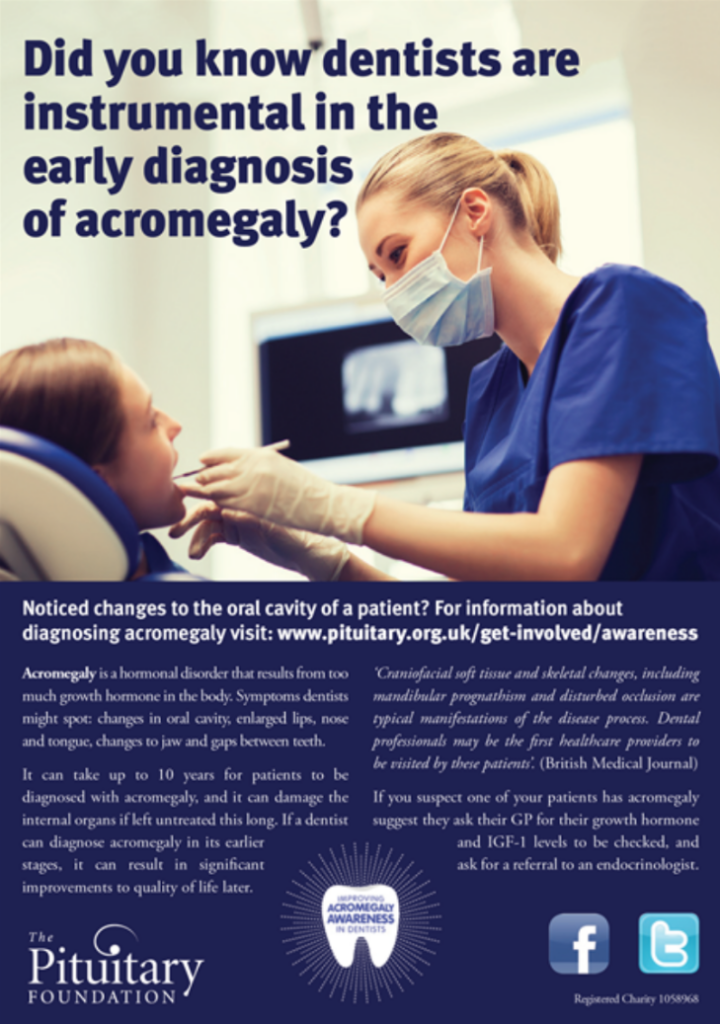
We ran a social media awareness campaign which reached over 60,000 people. Including publicising stories from patients who were diagnosed by their dentist. We targeted organisations working in the field of dentistry, and publicised our campaign materials including awareness leaflet. Approximately 2700 copies of the leaflet were circulated.
We also encouraged our members and volunteers to help spread awareness to their dentists.
We encouraged Dentists to look for changes to a patients oral cavity, and if this had changed, suggest they ask their GP for their growth hormone and IGF-1levels to be checked, and ask for a referral to an endocrinologist.
Campaign Facts
Acromegaly is a hormonal disorder that results from too much growth hormone in the body. Symptoms dentists might spot: changes in oral cavity, enlarged lips, nose and tongue, changes to jaw, and gaps between teeth.
It can take up to 10 years for patients to be diagnosed with acromegaly and it can damage the internal organs if left untreated this long. If a dentists can diagnose acromegaly in its earlier stages it can result in significant improvements to quality of life later.
The diagnosis is often delayed as the symptoms develop gradually over time, and patients and families may not notice the changes.
Studies show that untreated acromegalic patients are more likely to suffer from diabetes, high blood pressure and heart problems with a reduced life expectancy compared to the normal population. These can be improved after successful treatment.
British Medical Journal states
Craniofacial soft tissue and skeletal changes including mandibular prognathism and disturbed occlusion are typical manifestations of the disease process. Dental professionals may be the first healthcare providers to be visited by these patients and thereby prove instrumental in early diagnosis’
Read full article here
Our Message
The key campaign message in this awareness drive to primary care (GPs etc.) is that Cushing’s symptoms can be a great mimic for other more common conditions that are regularly seen by GPs, such as obesity, menopause, depression, and hypertension.
The more GPs who are aware, the more patients can be diagnosed early and avoid the frustrations, and poor wellbeing, associated with along diagnosis. The Foundation contacted the Royal College of General Practitioners (RCGP), the Nursing Standard, The BMJ and worked beside the Society for Endocrinology to help raise this awareness.
We encouraged schools and businesses to hold “Go Orange” days and simultaneously raise awareness and spread the message about the symptoms of Cushing’s. As ever, getting involved can make a significant difference to how widely our Awareness Month message spreads across the UK and Republic of Ireland.
We continue to work to support the diagnosis and treatment of Cushings.
The last day of February
Rare Disease Day takes place on the last day of February each year. This year it will be on the 28th February. The main objective of the campaign is to raise awareness amongst the general public and decision-makers about rare diseases and their impact on peoples' lives.
Each year we celebrate rare disease day. There will be different ways of getting involved, from sharing photos on social media, attending an event, or sharing your story.
Rare Disease Day was launched by EURORDIS-Rare Diseases Europe and its Council of National Alliances in 2008.
Get involved!
There are lots of ways you can get involved in Rare Disease Day. You might want to share a photo to show solidarity with people living with a rare disease in your community! Share a photo with painted hands on social media using #RareDiseaseDay and tag @rarediseaseday. You can also find lots of downloadable materials to create your own content on the Rare Disease Day website.
Every year, thousands of events are organised around the world to mark the occasion of Rare Disease Day.
You could organise an event at work or with friends and family, throughout February, to raise awareness. Don't forget to share pictures and videos using #RareDiseaseDay.
Share your story
You can raise awareness about rare diseases and their impact on peoples’ lives by sharing your story of living with a rare disease or caring for someone that does. You can share your stories with us by emailing [email protected], or you can share them with Rare Disease Day on their website.
You can stay up to date with the latest news from this year’s Rare Disease Day campaign by following them on Facebook, Twitter and Instagram.
This campaign has shown without a doubt that many non-endocrine health care professionals do not know what DI is, and immediately confuse it with diabetes mellitus.
The campaign ‘No Need To DI’ reached over 70,000 people on our social media. We received 221 comments and our posts were shared by 722 and over 4.600 signed our petition to change the name.
We have seen devastating accounts, from loved ones of patients who lost their lives, because the HCPs involved did not understand what DI is, how it should be treated and how it should be monitored.
We continued to work with an incredible team of dedicated endocrinologists including Prof John Wass, Dr Malcolm Prentice, Dr Miles Levy, Prof Stephanie Baldeweg, Dr Helen Simpson, the Society for Endocrinology and others and are delighted that the name change is being adopted.
To have any new name of a medical condition recognised by HCPs and patients, there are steps we have to follow and a lot of communication to ensure everyone knows and understands the change. For a while both names will be used.
It is vital that people with conditions like adrenal insufficiency and diabetes insipidus feel safe going into hospital and able to trust they will receive the necessary treatment.
We hear too many stories of pituitary patients being denied their vital medications (e.g. hydrocortisone and desmopressin) when in hospital or A&E and it is unacceptable. These drugs should never be omitted
Due to the pandemic, the focus was not on physical leaflets, but digital interventions. We asked our whole community to use their social media- and their imagination – to get the message out!
We also asked patients to complete the inaugural Patient Care Survey, which was the largest survey ever undertaken in this area.
We were delighted to have the support of the Society of Endocrinology for this campaign.