Medically Fact Checked 01/08/2015
By Gail Weingartner, Area Co-ordinator for the Solent Support Group
I’d like to tell readers about how attending a meeting entitled ‘Getting Steroid Replacement Right & Minimising the Side Effects’ has changed my life. This was run by Professor Peter Hindmarsh in London in March 2015 with two subsequent meetings being held since that time. As the title says, this was about getting our steroid replacement right for us as individuals and has totally turned on its head, how we as pituitary patients have been advised is the optimum methodology for our daily hydrocortisone replacement.
I have been a pituitary patient since diagnosing myself in November 1992 and subsequently became a founding member of The Pituitary Foundation at the launch in 1994. Many readers know of my struggle over the years with what I have called my ‘blip’ days, which can be described as my body saying “enough is enough, I need to recharge my batteries”. I experience total fatigue together with a massive hangover-type feeling, without the enjoyment of a glass or two the night before! The only thing I can do is sleep, sleep, sleep (with a desire to keep eating) for anywhere between one day (best scenario) and four days (worst).
This has affected my life hugely, with time off work and being so unreliable socially, but most significantly, this has also had such an emotional impact. The frequency of this scenario had worsened over the years; sometimes weekly, fortnightly or if I was lucky, once a month.
For many years I have taken my hydrocortisone three times a day; the biggest dose (approx. 65%) immediately upon waking, 20% at midday and the final 15% at 5.30pm. I frequently had to increase the dose on a blip day, which sometimes helped, but at other times, that was me wiped out in bed yet again. I would still plan a social life with friends, partner and family but they increasingly realised that I quite often wouldn’t make the event, because of my blip days. I’ve missed out on lots of special occasions, but I’m preaching to the converted aren’t I? Lots of you understand exactly what I’m saying here. Apart from feeling bloody disgusting (excuse my language), this has made me feel worthless, useless and as if I should be trying harder to ‘keep going’. Of course I’ve tried to work through it lots of times, which occasionally has been successful but invariably, it’d be back to bed to yet again, sleep, sleep, and more sleep.
Any improvement on the above would have been welcome but I couldn’t have imagined my quality of life could actually improve so much.
So, back to that amazingly interesting day with Prof Hindmarsh, which was about exploring the side effects of steroid therapy, how cortisol replacement can be measured and methods for improving treatment. From when I first heard about this meeting, it was stressed that this was for congenital adrenal hyperplasia, Addison’s and pituitary patients and importantly, for ADULTS as well as children. I want to reiterate that this is for both children and adults, because approximately 18 months ago, when I only had a little information about this methodology and shown it to an endocrinologist, she dismissed it very condescendingly saying it was only for children!
New regime
I have described my old hydrocortisone replacement routine and will come to my new regime shortly. Firstly, I want to make it absolutely clear that there is of course, the science behind this “working towards a single gold standard care protocol for all (including adult care) with adrenal insufficiency”, which was fully explained by Prof Peter Hindmarsh during his presentation. But, I won’t be attempting to do that here because I’m not qualified or indeed informed enough, to do so.
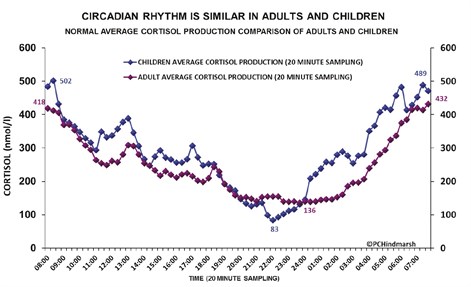
Graph 1: showing circadian rhythm is similar in adults & children.
Here though is a circadian rhythm graph showing how cortisol production is similar in both adults and children who produce the hormone in the normal way (lucky them!) You will see from this that in the early hours of the morning (1am) the production of cortisol starts to steadily rise with it peaking at approximately 6.30am. Wouldn’t it be fantastic if we could truly mimic how our bodies would naturally produce cortisol with our doses of hydrocortisone? At the presentation we learnt that, and I quote, “Hydrocortisone has a quick onset and the cortisol peaks to the highest level usually around one to two hours after being taken. The cortisol obtained from the tablet lasts in the blood circulation between four to six hours.” Research has also shown that the range for 50% of the dose to be used up in different people can be anywhere between 40 – 225 minutes. So, just having a single blood cortisol measurement or the cortisol day curve taken over several hours in hospital (not even over 24 hours) is unlikely to show where the individual falls between these two extremes. Dosing needs to be tailored to the individual and cortisol lasts differently depending upon the time of day.
With my old hydrocortisone routine, where I was taking my final dose at approximately 5.30pm, it makes sense that the cortisol would have been slowly depleting in my blood circulation and then from perhaps 11.30pm onwards, there would be little, if any cortisol, in my body until taking my morning dose around 6am. Is it any wonder I was getting up, feeling like a zombie until the hydrocortisone kicked in and then quite often, probably because I was so depleted anyway, the hydrocortisone never actually managed to bring my cortisol up to the level required to make me feel anywhere approaching normal. Below is a further graph showing this.
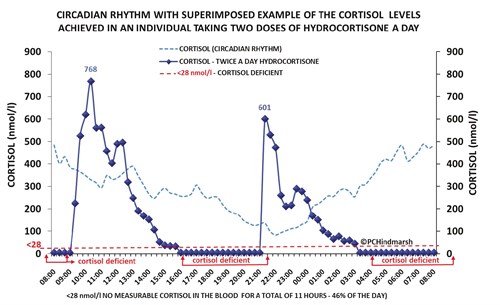
Graph 2: showing circadian rhythm with superimposed example of the cortisol levels achieved in an individual taking two doses of hydrocortisone a day.
Larger amounts than necessary
This is quite a complicated graph, but it does illustrate the fact that for considerable periods of time the patient is either receiving larger amounts of cortisol than is necessary or there are periods of time when the individual is under-replaced or totally cortisol-deficient.
After leaving the meeting, my sister Joy and I took the Underground to Waterloo to travel home and, using this remarkable information presented to us by Prof Hindmarsh (which now makes total sense), Joy devised my current hydrocortisone regime.
Bearing in mind and I quote once again “The cortisol obtained from the tablet lasts in the blood circulation between four to six hours” and also taking into account that we learnt how cortisol is inactivated by chemical changes that generate removal from the body in urine and faeces, my normal hydrocortisone dose is now split into six doses over each 24 hour period. I have NOT increased my daily dose, I am just taking the same overall daily dose more frequently; I view this as a drip feed effect, which is shown in approximate percentages below:
- 3am = approx. 22%
- 7am = 42%
- 11am = 15%
- 3pm = 7%
- 7pm = 7%
- 11pm = 7%
Are you wondering if taking hydrocortisone at 7pm, 11pm and 3am in the morning is affecting my sleep? I would say my sleep is probably better, even though it is a pain in the botty woken up by alarm at 3am, I usually turn over and go straight back to sleep.
Positives
The positives of my new regime far outweigh the one negative 3am dose, in that I have more energy, stamina and my quality of life has improved far beyond my expectations. Yes, I still experience blip days but they are not so frequent and (I hardly dare tempt fate by saying this) are only lasting for a single day before I bounce back. Writing this makes me feel quite emotional because life has improved so much and it is all down to that meeting presented by Professor Peter Hindmarsh back in March.
Copyright graphs reproduced with kind permission of Professor Peter Hindmarsh & Kathy Geertsma.
References:
www.cahisus.co.uk
www.cahisus.co.uk/leaflets.htm







